Key issues in decision making for gender transition treatment: Questions & Answers.

By Professor Dianna Kenny, PhD
In this article, I address key issues in the transgender debate as they pertain to children and young people. These include: Are “gender transition treatments” safe, “curative” and in the child’s best interest? In considering these questions, I explore the known negative consequences of puberty suppression and cross-sex hormones, including infertility and other medical conditions and the purported increase in suicidality without treatment. Can children and young people give truly informed consent to these interventions? What role should parents play in decision-making? On what basis are decisions made to proceed to gender transition? Are the foundations of such decisions logical and scientific? and What social forces are at play in this decision-making process?
1) Safety: Does the current scientific evidence support a conclusion that the administration of Gender Transition Treatment (social transition, puberty blocking agents and cross-sex hormones) can be safe for children and adolescents?
Answer: No. The metabolic implications of cross-sex hormone administration and the health effects of hormone manipulation on the bone, muscle, cardiovascular risk, cognition, and quality of life are not well understood (de Souza et al., 2017). Most of the research on health risks of cross-sex hormones have been undertaken on MTF (male‐to‐female) as compared to FTM (female-to-male) transsexuals. This has resulted in insufficient research on the effects of testosterone on FTMs (Newfield, Hart, Dibble, & Kohler, 2006). However, the effects of cross-sex hormones are not neutral for either group, as the literature surveyed below indicates.
The Effects of Hormonal Gender Affirmation Treatment on Mental Health in Female-to-Male Transsexuals
Surgical castration of male animals, leading to a loss of testosterone, results in marked decreases in synaptic density in the hippocampus and reductions in the capacity for learning and memory. FTM cross-sex hormone treatment results in loss of
bone mineral density (van Kesteren, Lips, Gooren, Asscheman, & Megens, 2001). Venous thrombo‐embolism (Asscheman, et al. 2014) and osteoporosis (Wierckx, 2012) have been identified as complications of cross‐sex hormone treatment of MTF transsexual patients. In a study of transwomen stratified by levels of circulating testosterone, those with the highest levels had the highest incidence of hepatic steatosis (fatty liver) and insulin resistance (Nelson et al. 2016).
Cross-sex hormone treatment may also be associated with hormone-related cancer, a risk that increases with duration of exposure and the aging of the transgender population (Mueller & Gooren, 2008; Quinn et al., 2015). Although the rate of ovarian cancers in FTM transsexuals is not known, several case studies have been reported in the literature, leading to the caution that testosterone treatment may be associated with increased risk of both ovarian and endometrial cancer (Izon, Tejada-Berges, Koelliker, Steinhoff, Granai, 2006). FTM transsexuals who do not proceed to total hysterectomy and bilateral salpingo-oophorectomy are at risk for endometrial, ovarian and cervical cancer (Menvielle & Gomez-Lobo, 2011). Other cancers e.g., (colorectal, lung, lymphatic and haematopoietic, and melanoma) do not appear to be elevated in the TF population compared with the RF group (Quinn et al. 2017).
A significantly higher prevalence of venous thrombosis, myocardial infarction, CVD (cardiovascular disease), and type 2 diabetes was found in trans females (TF) than in a control population (Wierckx et al., 2013). In the Quinn et al. (2017) study, myocardial infarction occurred at twice the rate in TF (1.8%) compared with reference females (RF) (0.9%). Peripheral artery disease (3.1% vs 1.9%) and unstable angina (1.8% vs 1.0%) were also elevated in TF compared with RF (Burcombe, Makris, Pittman, & Finer, 2003). In MTF transsexuals, high estrogen levels need to be avoided to prevent thrombosis, liver dysfunction and the development of hypertension. Up to 20% of MTF treated with estrogens show elevations in prolactin and pituitary enlargement (Menvielle, & Gomez-Lobo, 2011). These issues need constant, lifelong monitoring.
Bilateral mastectomy in FTM transgender patients carries substantial risks of surgical and medical complications. In one study of 57 FTM patients (40.4% of whom had comorbid psychiatric diagnoses), 33% experienced complications including hematoma, infection, seroma, fistula, or partial necrosis of the nipple-areola complex and 9% needed further corrective surgery, mostly for hematoma. A large population survey of TMs reported a higher risk for breast cancer, cervical cancer and smoking- and viral infection–related cancers (Silverberg et al., 2015).
Pubertal sex hormones affect brain development. For example, testosterone is associated with changes in cortical thickness, and estradiol is associated with grey matter development in girls.
With respect to psychological effects of cross-sex hormones, FTMs experienced more aggressive and sexual feelings and lower affect intensity after hormone administration (Slabbekoorn, 2001). Other personality characteristics such as empathy (higher in females) and aggression (higher in males) are associated with pre-natal testosterone exposure (Hines, 2008).
References:
Asscheman, H., T’Sjoen, G., Lemaire, A., Mas, M., Meriggiola, M. C., Mueller, A., & Gooren, L. J. (2014). Venous thrombo‐embolism as a complication of cross‐sex hormone treatment of male‐to‐female transsexual subjects: A review. Andrologia, 46(7), 791-795. doi: 10.1111/and.12150.
Burcombe, R.J., Makris, A., Pittam, M., Finer, N. (2003). Breast cancer after bilateral subcutaneous mastectomy in a female-to-male trans-sexual. The Breast, 2, 4, 290-293.ISSN 0960-9776,
Breast cancer after bilateral subcutaneous mastectomy in a female-to-male trans-sexual.
De Souza Santos, R., Frank, A. P., Nelson, M. D., Garcia, M. M., Palmer, B. F., & Clegg, D. J. (2017). Sex, Gender, and Transgender: Metabolic Impact of Cross Hormone Therapy. In F. Mauvais-Jarvis (Ed.), Sex and Gender Factors Affecting Metabolic Homeostasis, Diabetes and Obesity (pp. 611-627). Cham: Springer International Publishing.
Sex, Gender, and Transgender: Metabolic Impact of Cross Hormone Therapy.
Hines, M. (2008). Early androgen influences on human neural and behavioural development. Early Human Development, 84(12), 805-807. doi:
Early androgen influences on human neural and behavioural development.
Izon D. S, Tejada-Berges T, Koelliker S, Steinhoff M, Granai C, O. (2006). Ovarian cancer associated with testosterone supplementation in a female-to-male transsexual patient. Gynecol Obstet Invest; 62:226-228. doi: 10.1159/000094097
Ovarian cancer associated with testosterone supplementation in a female-to-male transsexual patient.
Kääriäinen, M., Salonen, K., Helminen, M., & Karhunen-Enckell, U. (2017). Chest-wall contouring surgery in female-to-male transgender patients: A one-center retrospective analysis of applied surgical techniques and results. Scandinavian Journal of Surgery, 106(1), 74-79.
Chest-wall contouring surgery in female-to-male transgender patients:
Menvielle, E., & Gomez-Lobo, V. (2011). Management of children and adolescents with gender dysphoria. Journal of Pediatric and Adolescent Gynecology, 24(4), 183-188. doi:
Management of children and adolescents with gender dysphoria.
Mueller, A., & Gooren, L. (2008). Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. European Journal of Endocrinology, 159, 197-202.
Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones.
Nelson, M.D., Szczepaniak, L. S., Wei, J., Szczepaniak, E., Sánchez, F. J., Vilain, E., Stern, J. H., Bergman, R. N., Bairey Merz, C. N., & Clegg, D. J. (2016). Transwomen and the metabolic syndrome: Is orchiectomy protective? Transgender Health, 1, 165–171.
Transwomen and the metabolic syndrome: Is orchiectomy protective?
Newfield, E., Hart, S., Dibble, S. and Kohler, L. 2006. Female-to-male transgender quality of life. Quality of Life Research, 15: 1447–1457.
Female-to-male transgender quality of life.
Quinn, V. P., Nash, R., Hunkeler, E., Contreras, R., Cromwell, L., Becerra-Culqui, T. A., . . . Goodman, M. (2017). Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open, 7(12), e018121. doi: 10.1136/bmjopen-2017-018121
Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people.
Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, Kanetsky PA, Schabath MB CA (2015). Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. Cancer J Clin. 2015 Sep-Oct; 65(5):384-400.
Silverberg, M. J., Nash, R., Becerra-Culqui, T. A., Cromwell, L., Getahun, D., Hunkeler, E., … & Roblin, D. (2017). Cohort study of cancer risk among insured transgender people. Annals of epidemiology, 27(8), 499.
Cohort study of cancer risk among insured transgender people.
Slabbekoorn, D., van Goozen, S., Megens, J., Gooren, L. and Cohen-Kettenis, P. 2001. Effects of cross-sex hormone treatment on emotionality in transsexuals. The International Journal of Transgenderism, 5(3) Retrieved from
Effects of cross-sex hormone treatment on emotionality in transsexuals.
Van Kesteren, P., Lips, P., Gooren, L., Asscheman, H., & Megens, J. (2001). Long‐term follow‐up of bone mineral density and bone metabolism in transsexuals treated with cross‐sex hormones. Clinical Endocrinology, 48(3), 347-354.
Wierckx, K., Elaut, E., Declercq, E., Heylens, G., De Cuypere, G., Taes, Y., . . . T’Sjoen, G. (2013). Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: A case-control study. European Journal of Endocrinology, 169(4), 471-478. doi:10.1530/EJE-13-0493
Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy.
2) Fertility: What are the implications for the fertility of children and adolescents following Gender Transition Treatment?
Answer: Puberty blocking agents (PBA) lower testosterone and estrogen to below normal levels, thus arresting normal puberty. There are no high-quality studies on the short and long-term effects of puberty-blocking agents. Continued suppression of puberty maintains male and female gonads (i.e., sex organs) in a state of immaturity. The addition of cross-sex hormones does not reverse this situation. This combination of drugs renders children infertile.
Prolonged exposure of the testes to estrogen risks irreversible testicular damage, therefore preventing future fertility (Hembree et al., 2009). Thus, cross-sex hormone therapy may result in partial to total impairment of spermatogenesis. GnRH analogs or depot-medroxyprogesterone used to stop menses prior to testosterone treatment. It is important to discuss with the family that there may be temporary or permanent decreased fertility.
Nonetheless, between 40%-50% of transgender adults surveyed reported a desire to have children and half of these wanted their own biological children (Jones, Reiter, & Greenblatt, 2016). Infertility is a very major risk associated with the application of puberty blocking agents and cross-sex hormones to children and young people. So high is this risk that gender clinics are attempting to develop fertility preserving methods for prepubertal children before commencing treatment. These methods are by no means fail safe but the interesting finding is that very few young people take up the option to preserve their fertility (Nahata, Tishelman, Caltabellotta, & Quinn, 2017). This suggests that they are not at the appropriate developmental level to be thinking so far into the future about prospective parenthood. Most children and adolescents attending gender clinics are in an egocentric phase of development and are not ready or able to make long term decisions.
The American College of Pediatrics has concluded:
Affirmation of children’s thoughts which are contrary to physical reality; the chemical castration of these children prior to puberty with GnRH agonists (puberty blockers which cause infertility, stunted growth, low bone density, and an unknown impact upon their brain development), and, finally, the permanent sterilization of these children prior to age 18 via cross-sex hormones… constitutes child abuse:
American College of Paediatrics Says Gender Ideology Hurts Children.
References:
Abel, B. S. (2014). Hormone treatment of children and adolescents with gender dysphoria: an ethical analysis. Hastings Center Report, 44(s4), S23-S27.
Hormone treatment of children and adolescents with gender dysphoria: an ethical analysis.
Hembree, W. C., Cohen-Kettenis, P., Delemarre-Van De Waal, H. A., Gooren, L. J., Meyer III, W. J., Spack, N. persons: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 94(9), 3132-3154.
An Endocrine Society clinical practice guideline.
Jones, C. A., Reiter, L., & Greenblatt, E. (2016). Fertility preservation in transgender patients, International Journal of Transgenderism, 17:2, 76-82, DOI:
Fertility preservation in transgender patients.
Michael Laidlaw, & Kevin Donovan (2019). The right to best care for children does not include the right to medical transition. The American Journal of Bioethics, 19:2, 75-77, DOI:
The right to best care for children does not include the right to medical transition.
Nahata, L., Tishelman, A. C., Caltabellotta, N. M., & Quinn, G. P. (2017). Low fertility preservation utilization among transgender youth. Journal of Adolescent Health, 61(1), 40-44.
3) Suicidality: In the case of a gender dysphoric young person experiencing suicidality, is the administration of Gender Transition Treatment, including pubertal suppression drugs and cross-sex hormones a reasonable or correct treatment for ameliorating suicidality?
Answer: Gender transition treatment does not lower the risk of suicide.
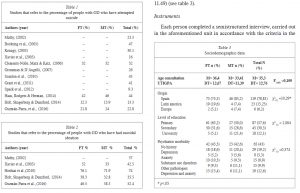
Although the suicide risk in this population is high, as the table below attests, there is scant research evidence that gender transition treatment results in lower risk for suicide. There is also a problem in studies on gender dysphoria and suicidality related to how suicidality is measured. Different rates will be obtained in different studies because of the use of different forms of measurement. For example, being asked if you have suicidal ideation will produce higher rates than counting the number of potentially lethal suicide attempts (Aitken, VanderLaan, Wasserman, Stojanovski, & Zucker, K. (2016).
GD Suicide Attempts and Ideation Tables.
Source: García-Vega, E. Camero, A., Fernández, M., & Villaverde, M. (2018). Suicidal ideation and suicide attempts in persons with gender dysphoria. Psicothema, 30, 3, 283-288 doi: 10.7334/ psicothema2017.438
Suicidal ideation and suicide attempts in persons with gender dysphoria.
Download pdf here> Suicidal ideation and suicide attempts in persons with gender dysphoria.pdf
(Click Here> To access an online PDF translator to your language.)
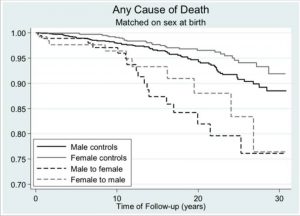
Although further robust longitudinal studies are needed, current evidence (Dhejne, Lichtenstein, Boman, Johansson, Långstrom, et al., 2011) indicates that those having undergone sex reassignment have significantly higher risk for mortality (3 times more likely), suicidality (5 times more likely), death by suicide (19 times more likely), and psychiatric morbidity (3 times more likely) than matched controls in the general population. Figure 1 shows the trends over a 30-year follow-up period. Negative outcomes were greater for MTF compared with FTM individuals. Transgender treatment does not prevent suicide, and may have other adverse effects on mental health post transition.
Any Case Of death Match On Sex at Birth Table.
Figure 1: Death from any cause as a function of time after sex reassignment among 324 transsexual persons in Sweden (male-to-female: N = 191, female-to-male: N = 133), and population controls matched on birth year [Source: Dhejne,
Lichtenstein, Boman, Johansson, Långstrom, et al. (2011)].
The vexed question is one of causality. Does gender dysphoria cause suicidality or is it the discriminatory treatment and social exclusion suffered by the transgender community that is causative, or are suicidality and gender dysphoria caused by
a third factor, such as mental illness, family dysfunction, parental or social factors? In my work with transgender adolescents, I have noted with great concern the serious underlying emotional disturbance in these young people who need intensive psychotherapy and parental and family therapy to resolve these disturbances. I wonder about those who go straight to gender clinics and gender affirming professionals who skate over these cracks in their personalities and social adjustment and proceed to gender transition in the naïve belief that this will resolve all of their presenting difficulties?
Reference:
Aitken, M., VanderLaan, D. P., Wasserman, L., Stojanovski, S., & Zucker, K. J. (2016). Self-harm and suicidality in children referred for gender dysphoria. Journal of the American Academy of Child & Adolescent Psychiatry, 55(6), 513-520. doi:
Self-harm and suicidality in children referred for gender dysphoria.
4) Child’s Best Interests: Are there circumstances under which the administration of Gender Transition Treatment could be in the best interests of children and adolescents?
Answer: If there are, they would be extremely infrequent.
According to the American College of Paediatricians (2018a):
Human sex is a binary, biologically determined, and immutable trait from conception forward. … “XY” and “XX” are genetic markers of male and female, respectively, and are found in every cell of the human body including the brain. Sex is established at conception, declares itself in utero, and is acknowledged at birth.
There are no objective (laboratory, imaging etc) or psychological tests that can reliably diagnose a “true transgender child.” By late adolescence, children with gender dysphoria who are allowed to experience natural puberty will come to accept their sex. Between 61%-98% of children desist from a transgender identity. One study of gender dysphoric boys (n=246) followed into adulthood showed that 84% spontaneously desisted. Most became either same-sex-attracted or bisexual (Singh, 2012). There is no way of predicting who will remain gender dysphoric. Therefore, 80-90% of children will be irreversibly harmed by gender transition therapy. Puberty blocking agents (PBA) derail the path of natural desistance – once children are placed on PBA, most, as adolescents, desire to progress to cross-sex hormones because of the physiological and/or psychological effects of PBA (Steensma et al., 2013).
According to the American College of Paediatricians (2018b):
Gender dysphoria (GD) of childhood describes a psychological condition in which children experience a marked incongruence between their experienced gender and the gender associated with their biological sex. When this occurs in the pre-pubertal child, GD resolves in the vast majority of patients by late adolescence. Currently there is a vigorous, albeit suppressed, debate among physicians, therapists, and academics regarding what is fast becoming the new treatment standard for GD in children. This new paradigm is rooted in the assumption that GD is innate, and involves pubertal suppression with gonadotropin releasing hormone (GnRH) agonists followed by… cross-sex hormones—a combination that results in the sterility of minors. …This protocol is founded upon an unscientific gender ideology, lacks an evidence base, and violates the long-standing ethical principle of “First do no harm.
Data on the persistence of the adolescent transgender lifestyle into adulthood is unreliable, primarily because so many are lost to follow up (Dhejne, Lichtenstein, Boman, Johansson, Långström, & Landén, 2011). Recent observations suggest that the rates of those wishing to de-transition are increasing.
Data on the persistence of the adolescent transgender lifestyle into adulthood is unreliable.
But any research or discussion on de-transitioning is being blocked by the transgender lobby and by professionals such as those in ethics committees in universities who fail to show any moral courage in supporting such research.
References:
American College of Paediatricians (2018a):
Download pdf here> Joint-letter-to-HHS-DOJ-DOE-Uphold-Definition-of-Sex
(Click Here> To access an online PDF translator to your language. )
American College of Paediatricians Speaks / Position Statement on Gender Dysphoria.
Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L., Långström, N., & Landén, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PloS one, 6(2), e16885. doi:10.1371/journal.pone.0016885
Long-term follow-up of transsexual persons undergoing sex reassignment.
Download pdf here> Singh, Devita (2012). A follow up study of boys with gender dysphoria.
(Click Here> To access an online PDF translator to your language. )
Steensma, Thomas D., et al. (2013). gender identity development in adolescence. Hormones and Behavior, 64, 2, pp.
288–297. doi:10.1016/j.yhbeh.2013.02.020.
Gender identity development in adolescence. Hormones and Behavior.
The new taboo: More people regret sex change and want to ‘detransition’, surgeon says
5) Informed Consent: Can children and adolescents understand the risks, benefits, and consequences of Gender Transition Treatment and give informed consent to it?
Answer: It is very difficult for anyone, particularly minors, to give consent to treatment for a fictitious condition. Further, a significant proportion of children and adolescents seeking such treatment have comorbid psychological, psychiatric, intellectual and cognitive disorders that preclude the capacity for informed consent.
Cases before the Family Court of Australia seeking court authorization for cross-sex hormone treatment or sex reassignment surgery have increased dramatically since 2004, which heard one case, to 18 cases in 2015, and 22 cases in 2016. In total, the court has ruled on 56 cases in this time period, including authorizing five young women for bilateral mastectomy. In these 56 children, 25 of 39 cases in which family constellation could be discerned lived in single parent families or foster care, with only 14 from two parent families. In this same group of 56 children, 50% had a diagnosed psychological disorder, including Autism Spectrum Disorder (ASD), major depression, anxiety, oppositional defiance disorder (ODD), ADHD, and intellectual disability. A recent study has shown a higher prevalence of gender dysphoria in those with ASD (van der Miesen, Hurley, Bal, & de Vries, 2018).
In a sample of 105 gender dysphoric adolescents and using the Diagnostic Interview Schedule for Children (DISC), anxiety disorders were found in 21%, mood disorders in 12.4%, and disruptive disorders in 11.4% of the adolescents. Males had greater psychopathology compared with females, including comorbid diagnoses (de Vries et al. 2011).
For some [children identifying as “transgender”], the major issue is cross-gender behaviour’s or identifications; for others, the gender issues seem to be epiphenomena of psychopathology, exposure to trauma, or attempts to resolve problems such as higher social status or other benefits they perceive to be associated with the other gender (Drescher & Byne, 2012, p.
503).
KEY ISSUES IN DECISION-MAKING FOR GENDER TRANSITION TREATMENT:
In the adult transgender population, mental health has also been found to be more impaired in the transgender population compared with male and female reference groups (Quinn et al., 2017). For example, anxiety was diagnosed in 38% of trans females (TF) compared with 22% of reference females (RF). Depression was diagnosed in 49% (TF) vs 25% (RF); suicidal ideation in 5% (TF) compared with 0.6% (RF); and substance abuse disorder in 15% TF compared with 5% RF. In trans males (TM) mental health was significantly worse compared with reference males (RM). For example, 46% TM were diagnosed with anxiety compared with 13% RM. Similarly, for depression (55% vs13%), self-inflicted injury (4.2% vs 0.4%), suicidal ideation (6.7% vs 0.6%), and substance abuse disorder (14% vs 8.4%), TM were significantly more disadvantaged than RM.
Informed consent can also be impeded by extraneous factors in the environment that “seduce” young people to adopt a particular stance without the full and conscious knowledge of how their thinking and feeling on the subject has been influenced. Given the strong evidence of peer contagion in suicide, substance abuse and eating disorders, especially among adolescents, the role of peer contagion in gender dysphoria demands urgent attention.
If we examine the gender dysphoria epidemic in social network terms, we see several features operating. It is an open-system network with nodes and ties expanding across the globe. Most countries are reporting sharp increases in the number of people seeking services and treatment for gender dysphoria. Many are ramping up services and setting up new gender clinics to cope with demand. This network is highly centralised with only one voice – the transactivist lobby advocating immediate gender transition treatment – being heard above the desperate whispers of terrified parents and horrified academics, researchers, doctors, psychologists and psychotherapists. Opinion leaders operating at the centre of these networks are very influential. The level of density in a network has two effects – firstly, it enhances the circulation of information between members and secondly, it blocks the introduction of dissenting ideas and evidence (Iyengar, Van den Bulte, & Valente, 2011). Most young people will deny that they are susceptible to such influences and that they have made up their own mind. However, when questioned, they repeat the slogans propagated by the trans-lobby as their reasons for wanting undergo gender transition treatment.
References:
De Vries, A. L., Noens, I. L., Cohen-Kettenis, P. T., van Berckelaer-Onnes, I. A., & Doreleijers, T. A. (2010). Autism spectrum disorders in gender dysphoric children and adolescents. Journal of Autism and Developmental Disorders, 40(8), 930-936.
Autism spectrum disorders in gender dysphoric children and adolescents.
Drescher, J., & Byne, W. (2012). Gender dysphoric/gender variant (gd/gv) children and adolescents: Summarizing what we know and what we have yet to learn. Journal of Homosexuality, 59(3), 501-510. doi: 10.1080/00918369.2012.653317
Iyengar, R., Van den Bulte, C., & Valente, T. W. (2011). Opinion leadership and social contagion in new product diffusion. Marketing Science, 30(2), 195-212.
Opinion leadership and social contagion in new product diffusion.
Quinn, V. P., Nash, R., Hunkeler, E., Contreras, R., Cromwell, L., Becerra-Culqui, T. A., . . . Goodman, M. (2017). Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open, 7(12), e018121. doi: 10.1136/bmjopen-2017-018121
Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people.
Van der Miesen, A. I. R., Hurley, H., Bal, A. M., & de Vries, A. L. C. (2018). Prevalence of the wish to be of the opposite gender in adolescents and adults with autism spectrum disorder. Archives of Sexual Behavior. doi: 10.1007/s10508-018-1218-3
6) Parental Role: Should a role be reserved for a mother or father in assisting their children to understand whether Gender Transition Treatment is right for them?
Answer: Definitely. In addition, there is a role for assessment of the parental dynamics, the parent-child relationship and the family constellation of gender dysphoric children before any decisions are made to proceed to treatment.
We need to investigate the context in which gender dysphoria arises and the reasons for the exponential increase in cases observed over the past decade, an increase tantamount to a psychic epidemic. These include family constellation, parental gendered behaviours and attitudes, child maltreatment, and peer contagion and cultural factors.
Gender dysphoria might be better understood as a relational process rather than as an inherent property of the individual. Illuminating the interactional dynamics in which young children assert that they are transgender rather than unthinkingly affirming their cross-gender assertions is confronting for all concerned, including parents, doctors, therapists, and transactivists.
Studies in the developmental psychology literature about factors that influence gender development in traditional families.
(McHale, Updegraff, Helms-Erikson,& Crouter, 2001;
Sumontha, Farr, & Patterson, 2017;
can inform and guide research into families with a transgender child. There is an emergent literature on gender dysphoria that is exploring family dynamics, the interpersonal quality of parent-child.
(Zucker, Wood, Singh, & Bradley, 2012)
and sibling
(Rust, Golombok, Hines, Johnston, & Golding, 2000)
relationships and parental gender attitudes and behaviours
in families with a transgender child
(Riley, Sitharthan, Clemson, & Diamond, 2011)
although the literature is still sparse in this respect.
KEY ISSUES IN DECISION-MAKING FOR GENDER TRANSITION TREATMENT: Questions and answers
One study of traditional families found that preadolescent children who are anxiously attached to their mothers or who had a preoccupied form of insecure attachment to their mothers experienced lower gender contentedness and fewer gender-typical feelings compared with securely attached children
What effect would a parent who preferred a child of the opposite sex have on a child’s gender identity? Such a question could usefully be explored in families with a transgender child.
“Parents are critical mediators of the experiences of their gender variant children…” (Gray, Sweeney, Randazzo, & Levitt, 2016, p. 123),
KEY ISSUES IN DECISION-MAKING FOR GENDER TRANSITION TREATMENT.
as indeed are siblings, peers, and the wider ecological context in which children grow and learn, including gender clinics, social media, and purported experts. The influence of all these factors on the gender dysphoric child are not well understood. Accordingly, great care needs to be exercised and thorough assessments conducted before making irreversible changes to their developing bodies.
In addition, parents are subject to the same influences as their declared transgender children. They are constantly trawling the internet, joining parent support groups, giving media interviews espousing clichés in which they have been schooled by gender clinics of the kind, “I would rather have a live trans daughter than a dead son.” Parents may have their own psychopathologies that are playing out in the transgender drama of their children. For separated parents, it often becomes a battleground in which one supports their child’s declared gender identity while the other struggles to prevent the administration of harmful drugs and mutilating surgery. Such families need to be assessed for parental alienation.
7) Faulty logic: What are the assumptions underpinning the understanding of the gender dysphoria in transactivist lobbies?
Answer: Transgender advocates state that in transgenderism – the belief/assumption that one has been born in the wrong body – the body must be aligned to one’s gender belief, not one’s belief to one’s biological body. They assume that the mind is “correct” in its perceptions and beliefs and the body is diseased and must be treated. Transgenderism is a disorder of assumption and like other disorders of assumption, is solipsistic. Solipsism is the belief that ideas that arise in the mind are true and cannot be questioned. For example, those with anorexia nervosa believe that they are a fat when in fact they are emaciated. People with body image dysmorphia engage in endless plastic surgery to correct their perceived ugliness, when their appearance falls well within the ‘norms’ for their culture. Those with body integrity identity disorder (BIID) perceive one or more of their normal limbs or organs as alien to the rest of their body and wish to have it (them) removed, amputated or paralysed. If refused surgery, they may self-mutilate. Can we, as a society, condone the amputation or paralysis of healthy limbs in people with BIID? In the same vein, is the amputation of a healthy penis and healthy breasts ethically justifiable? Disorders of assumption are disorders of perception. Disorders of perception belong in the domains of psychology, psychiatry, and psychotherapy, not endocrinology or mutilating surgery.
In the Middles Ages, the belief that some women were “witches” resulted in the murder of thousands of innocents during the Inquisition. More recently, families were torn apart by the “recovered memories” epidemic. Innocent teachers spent many years in jail after false accusations of “ritual sexual abuse” at preschools (Kenny, 2015). If transgender hysteria is not stemmed, it will result in the devastation of the lives of young people who get swept up in the cause of gender transition. Many may change their minds, but sex reassignment surgery and sterility as a result of cross-sex hormone treatment are generally irreversible.
God, Freud and Religion. The origins of faith, fear and fundamentalism.
McHugh (2008; 2014) argued, “Sex change is biologically impossible. People who undergo sex-reassignment surgery do not change from men to women or women to men. Rather, they become feminized men or masculinized women”
Former Johns Hopkins Head Psychiatrist. Transgender Surgery Isnt The Solution
8) Social Factors: What are the social forces propelling the gender dysphoria pandemic?
Answer: Social contagion and group think.
Contagion is a biological concept originating in the field of epidemiology. It describes the pattern of dissemination across networks of a disease, allowing patterns and causes of contagion to be identified and tracked. The concept has been borrowed by the social sciences to understand fads, politics, financial behaviour, and the popularity of new theories.
A related concept is groupthink. Groupthink, a term coined by social psychologist Irving Janis (1972), is an extreme form of conformity in which people are prepared to keep the peace at all costs. It tends to occur more in homogenous groups, when a powerful and charismatic group leader is insistent on the preferred course of action, when the group is under severe stress, where significant moral dilemmas are part of the decision matrix and where objective outside experts are not called upon. The consequences of group think include the illusion of invulnerability, collective rationalization, stereotyping of out-groups, self-censorship, belief in the inherent morality of the group, poor information search, incomplete survey of alternatives, failure to appraise the risks of the preferred solution, selective information processing, and conflation of ethics and expedience.
Transgender hysteria. (Kenny, 2015; Turner & Pratkanis, 1998).
Transgenderism is primarily a sociocultural and political phenomenon, not a psychological or medical reality that has been fuelled by both social contagion and groupthink social processes. One can observe all the features described above in the conduct of transgender advocacy groups.
References:
Download pdf here> Janis, I.L. (1972). Victims of groupthink: A psychological study of foreign-policy
decisions and fiascos. Boston: Houghton Mifflin.
(Click Here> To access an online PDF translator to your language. )
(Click Here> To access an online PDF translator to your language. )